Early diagnosis is key to stopping the spread of tuberculosis (TB)
Despite progress in diagnosis and treatment, tuberculosis continues to claim thousands of lives each year – more than HIV and malaria combined. AIDS Healthcare Foundation South Africa (AHF) is calling for urgent and coordinated action to accelerate TB prevention, improve diagnosis and treatment, and strengthen the country’s response to drug-resistant TB (DR-TB).
According to the World Health Organization (WHO), TB claimed 1.25 million lives globally in 2023. Multidrug-resistant TB (MDR-TB) remains a serious public health crisis, with only two in five people receiving treatment for drug-resistant tuberculosis in 2023.
TB cases continue to rise
Nearly 11 million people fell ill with the disease last year, with more than 80% of cases and deaths occurring in low- and middle-income countries like South Africa. While the global incidence of TB is declining, progress is far too slow and inconsistent to meet international targets.
An estimated $22 billion is needed annually to end TB (World Health Organization) if we are to end TB by 2027 – less than 48 months from now, yet global funding continues to fall short, prompting a need to address governments on innovative funding models to strengthen Domestic Resource Mobilization.
Relying only on existing health financing models without exploring innovative health financing solutions undermines South Africa’s ability to sustain an effective TB response. Addressing TB requires significant investment from national health budgets, which are already under strain. Yet, opportunities such as public-private partnerships (PPPs) remain underutilised in the health sector.
“Public-private partnerships are a vital tool for health financing because they leverage private sector resources, expertise, and efficiencies to complement government efforts, expanding access to services and improving health outcomes,” explains Ngaa Murombedzi, Regional Advocacy and Policy Manager (Southern Africa) at AHF.
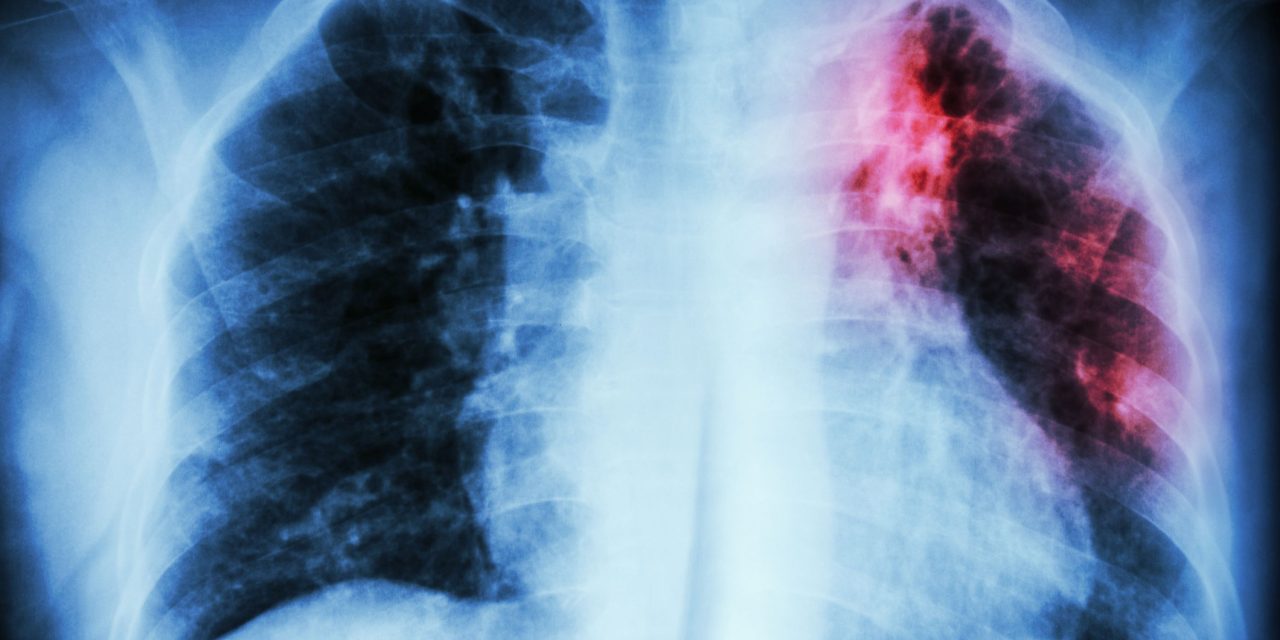
Strengthening early detection and diagnosis
Early diagnosis is key to stopping the spread of TB. While South Africa has expanded the use of molecular diagnostic tools like the GeneXpert MTB/RIF test, more than 65 000 TB cases were missed in 2022 – many among young people aged 15–24 and adults over 65.
“Despite having advanced technologies, screening and diagnostic protocols are not fully applied at primary healthcare level,” says Dr. Maxime Molisho, Provincial Medical Manager for AHF Mpumalanga. “We need to ensure that clinicians are properly trained to use tools like chest X-rays with computer-aided detection (CAD), urine LAM testing, and effective referral systems.”
AHF is addressing these gaps by deploying clinicians to its supported facilities and providing ongoing training on TB screening, diagnosis, and clinical management. “Patients with late-stage HIV are screened early to ensure timely diagnosis and care,” says Mmatsie Tsotetsi, Advocacy Manager at AHF South Africa.
Tackling drug-resistant TB
In 2022, South Africa reported approximately 11 000 DR-TB cases, with more than 6 700 confirmed as MDR-TB. Poor treatment adherence, interruptions in medication, and incorrect dosing are contributing factors.
The WHO’s updated guidelines offer hope. The shorter six-to-nine-month BPaLM treatment regimen – combining bedaquiline, pretomanid, linezolid, and moxifloxacin – has improved treatment success rates to over 60%.
However, challenges remain in ensuring patients complete their treatment. “Through telephonic follow-ups, food support for eligible patients, and partnerships with community organisations, AHF is working hard to reduce treatment drop-outs and improve outcomes for DR-TB patients,” adds Dr. Nxele.
A comprehensive approach to TB care
AHF continues to prioritise integrated HIV/TB care across its clinics. TB prevention, screening, and treatment are essential components of AHF’s global healthcare programs. AHF also advocates for policies that make TB drugs and diagnostic tools more accessible and affordable, while actively engaging communities and governments in the fight against tuberculosis.
In KwaZulu-Natal, AHF supports the Stop TB in Children campaign, aimed at increasing screening among school-going children and those outside the education system.
In Gauteng, the focus is on addressing the social determinants of health, such as nutrition, access to social services, and identity documentation, through partnerships with departments like Social Development, SASSA, and Home Affairs.
“We must take collective responsibility,” says Dr. Kgomotso Thipe, AHF Gauteng Provincial Medical Manager. “TB is airborne, highly infectious, and preventable, but only if we act decisively. Early detection, community awareness, and breaking the stigma are critical to saving lives.”
Sources
Op-ed by: AIDS Healthcare Foundation (AHF).